The #StayHome is being one of the most important weapons in the fight against the COVID-19 health crisis. I believe that any trick or recommendation to best cope, physically and mentally, with this home confinement is always welcome. Therefore, here is my bit to try to help all of you who have some degree of leg edema because the venous and/or lymphatic return is not adequate.
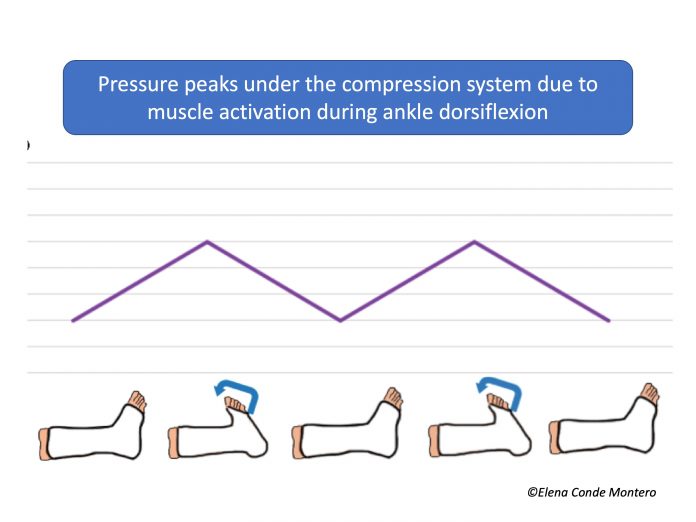
Compression therapy is the mainstay of treatment for venous hypertension, but it should always be associated with physical exercise (adapted to the situation of each person) and anti-edema measures (essentially rest with elevated lower limbs), as we saw in the post “Essential Decalogue in the fight against venous hypertension“. In the blog entry “Phlebolymphedema, a term that should more frequently used” we explained the need for physical exercise to activate the plantar and calf pump, and thus promote venous and lymphatic circulation. As we also commented in the post “Band and bandage: not the same thing“, the higher the stiffness index of the compression system used, the more effective it will be in resisting muscle contraction and achieving high pressure peaks that create brief and intermittent venous occlusions, similar to the physiological functioning of the valves. As muscle contraction is so relevant, muscle atrophy or limited mobility may diminish the effectiveness of compression bandages.

So, if exercise is so important, now that we can’t go for a walk, what can we do at home to encourage venous return?
Young people, with few joint problems and good mobility, can do planned exercises, with or without apparatus (exercise bike), to activate the muscle pump of the calf and foot (let’s not forget that the plantar muscles are very important).
However, being old and having reduced mobility, in addition to other associated comorbidities, does not mean that it is impossible to activate the muscle pump. Here you can find some exercises for dorsal and plantar flexion of the ankle that you can do in a series, for example, of 20 repetitions several times a day, as long as you remember it. The ideal is to do them completely lying on your back, with your legs raised, supported by 2-3 cushions/pillows. If lying in bed is only possible at night, we will take advantage of this moment to do it this way and, the rest of the day, we can do it sitting up, with our legs elevated.

As we said at the beginning, anti-edema measures are fundamental, so we recommend keeping your legs elevated whenever you are sitting. If you have trouble difficulty keeping your legs elevated for a long time, which would be optimal, we can also do the following exercises to activate the muscle pump.

If, in addition to phlebolymphedema and immobility (wheelchair), there is also a certain degree of arteriopathy (ABI>0.5), high stiffness index bandages with pressures lower than 30 mmHg (or Velcro wraps) is a safe and effective option if the dorsiflexion and plantar flexion exercises we have just seen are performed.
Before finishing, remember that these exercises also help maintain or improve the flexibility of the ankle joint, which is fundamental for the proper functioning of the plantar and calf muscle pump during walking (“Improving the calf pump using home-based exercises for patients with chronic venous disease”).
I am taking this opportunity to send you all a big hug. The wound clinic will be closed for a while, but anything that can be resolved telematically, do not hesitate to consult me. The next few weeks my work will be very different from usual and I will have a new team, made up of exceptional professionals, who are extremely supportive and who give their best every day to help people with COVID-19. Take care of yourselves 🙂