Enzymatic debridement is a widely used technique. However, many professionals are strongly opposed to this type of debridement. The objective of this post is to clarify the mechanism of action of the different enzymes used in the wound bed, their potential benefits and the limitations they present. Before we start, I would like to thank the great expert Carmen Alba Moratilla for having proposed me to deal with this subject. I would love to share her opinion and experience with everyone, which will be very enriching and can be considered as the second part of this post.
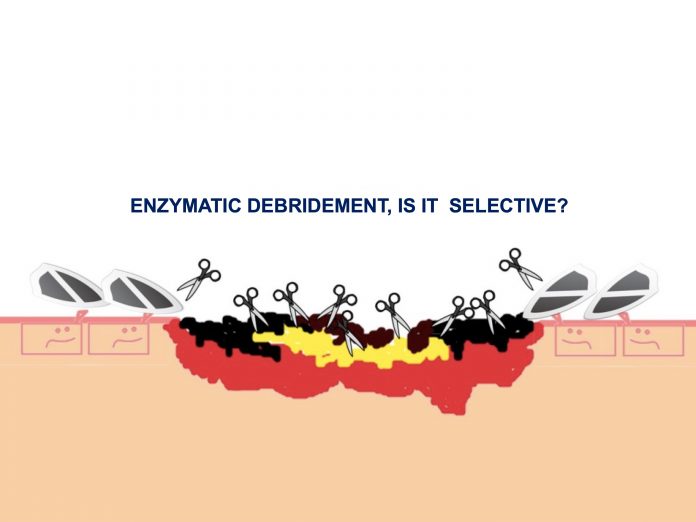
In any wound, the presence of non-viable tissue represents an impediment to the formation of adequate granulation tissue and creates a favorable environment for bacterial proliferation, thus maintaining an abnormally prolonged inflammatory phase. The different debridement techniques aim to destroy or remove this tissue to redirect the wound healing process. Enzymatic debridement is characterized by the use of proteolytic enzymes aimed at degrading the denatured proteins in the wound bed. The selectivity of debridement will vary depending on the enzyme used. In order not to damage healthy tissue, the highest possible specificity is required. Therefore, proteases with a broad spectrum of action (they bind to combinations of amino acids that are present in multiple proteins, including growth factors), such as papain (extracted from papaya), are methods that should no longer be used.
Now we will explain the enzymatic agents that are used in our clinical practice for wound debridement:
- Collagenase: it is the most widely used enzyme. It can be obtained from different bacteria. The one used in the most common commercial preparation available in our country is obtained from the purified filtering of the Clostridium histolyticum culture. It is characterized by a selective degradation of collagen, with low fibrinolytic activity, so it would not increase the risk of bleeding in wounds.1There are different types of collagen in the body. The in vitro activity of collagenase has been shown against different types of collagen, including type I and III helical collagen fibres, which are present in the dermis.1On the other hand, in vitro studies have shown that, like some metalloproteinases found in wounds in a physiological way, collagenase and the products obtained from collagen degradation promote the proliferation and migration of keratinocytes and fibroblasts. Based on this finding, some authors recommend their use both in the initial debridement phase and in the maintenance phase, when non-viable tissue is no longer visible.1
But how does collagenase distinguish denatured collagen fibres from viable ones? I have only found one reference to this, which suggests that this enzyme would not recognise its attachment points in healthy collagen because it is covered and protected by mucopolysaccharidesina.2
- Urokinase, streptokinase: these are serine-proteases of human and bacterial origin, respectively, which facilitate the conversion of plasminogen to plasmin, in order to degrade fibrin. Because of their mechanism of action, they can promote bleeding. Since they act indirectly, their action depends on the amount of plasminogen present in the exudate
However, is it of interest to remove all the fibrin from the wound bed, and is collagen or fibrin the denatured protein that is found in greater quantity in a bed with slough and necrotic tissue? Studies indicate that the presence of denatured collagen clearly predominates over other proteins such as fibrin, elastin or fibronectin.
Now let’s go to the practical side: What do these products provide in our the day-to-day clinical practice?
Clinical trials to determine the benefits of enzymatic debridement are scarce and have focused on collagenase. The small number of patients and the limitations in their design stand out. One of these is a randomised, double-blind trial of 27 pressure ulcers in which debridement at 6 weeks was compared in the collagenase ointment group (13 patients) and the hydrogel group (14 patients).3 Total debridement was obtained in 85% of the wounds in the first group and 29% in the second. Another unblinded randomised controlled study was performed on 55 diabetic foot ulcers to compare isolated sharp debridement with combined use of collagenase at 6 weeks of treatment and at a 6 week follow-up.4 Of the variables studied (wound area, clinical appearance, number of sharp debridements needed, time to healing), only statistically significant differences in wound area reduction in favour of the collagenase treated group were found.
In my opinion, and I agree with other authors,5 regarding the usefulness of enzymatic debridement in clinical practice, the excipient of the product and the secondary dressings used, as well as the combined use of sharp debridement, play a key role in the results obtained. The promotion of a moist environment results in both exogenous and autolytic debridement (by the action of enzymes present in the wound in a physiological way). In this sense, the differences obtained in studies that compare the action of different collagenases in different excipients, which favour preparations that optimise the maintenance of the appropriate microenvironment and protect the perilesional skin (such as hyaluronic acid), are noteworthy.6
With regard to the combined use of different products, it must be taken into account that enzymes are proteins and, therefore, their activity depends on their conformation and on having a free binding site with other proteins. Combination with iodized preparations or silver dressings decreases the activity of collagenase and should therefore be avoided.6
References: