Many of the ulcers we may find in our daily clinical practice develop in the context of a post-thrombotic syndrome. It is important to know this entity, which has an important impact on the quality of life of patients and on health costs.
What is the post-thrombotic syndrome?
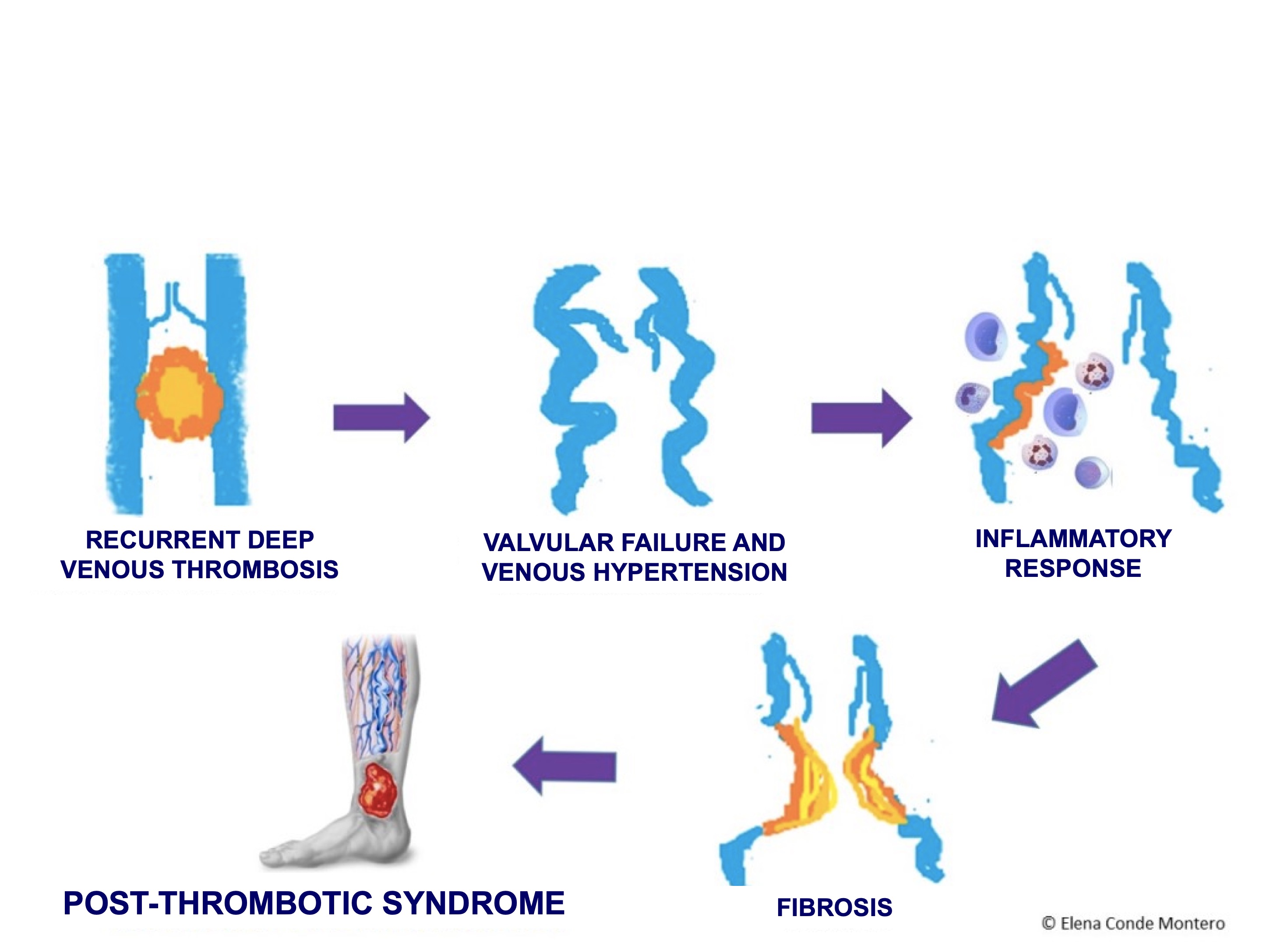
It is a long-term complication of deep vein thrombosis (DVT). Repeated episodes of DVT are a clearly established risk factor. It is the result of venous hypertension that develops due to valvular incompetence, reflux and/or venous obstruction, with an associated alteration in microcirculation. After the thrombotic episode, there is a weakening of the venous wall, with incomplete valve closure, reflux and secondary venous hypertension. Endothelial distension occurs, with increased wall permeability and chemotherapeutic effect on inflammatory cells, predominantly macrophages and leukocytes. The inflammatory process triggers a perivenous fibrosis and development of trophic alterations in the affected segment (See figure).
Its incidence is difficult to establish due to differences in follow-up time, patient selection and definition of post-thrombotic syndrome in the different studies. It is estimated that, one year after the occurrence of a deep vein thrombosis, up to 50% of patients will suffer post-thrombotic manifestations (Gabriel, 2003).
What are its clinical manifestations?
Among the signs that may be present, we find:
- Edema
- Tortuous veins
- Skin alterations due to stasis. Ulceration would be the extreme degree, but hyperpigmentation, eczema and hypodermitis are very frequent findings. The development of ulcers may be triggered by trauma or may appear spontaneously. They are characteristically chronic with a high rate of recurrence.
The most common symptoms are pain, itching and a feeling of heaviness. (Torres, 1995).
How is it diagnosed?
Diagnosis is made through clinical and complementary macrocirculatory tests (color Doppler ultrasound, phlebography and magnetic angioresonance) and microcirculatory ones (Doppler laser flowmeters, transcutaneous measurement of partial pressure of O2 and CO2 and impedance plethysmography) (Gabriel, 2003).
How is it treated?
Medical treatment:
In those patients without surgical indication (most of them), local treatment of the ulcer must be associated with other strategies that can promote healing. The most widely accepted and used is compression therapy.
As we commented before, the role of microcirculation alterations in this syndrome is as important as changes in macrocirculation. Therefore, different drugs have been used that act at that level, favoring an adequate blood flow.
My experience is satisfactory with the use of either pentoxifylline and sulodexide, associated with compressive therapy.
The usefulness of both drugs in the treatment of chronic venous ulcers is supported by the results of different studies. Pentoxifylline has haemorrheological properties (increases the malleability of the red blood cell membrane) and inhibits the adhesion of platelets and leukocytes to the endothelium (Jull, 2012). Sulodexide is an orally administered heparinoid with antithrombotic and fibrinolytic action (Andreozzi, 2012).
Interventional treatment:
Depending on the hemodynamic findings, there are cases that may benefit from an invasive intervention. Correction of reflux points and improvement of venous return pathways may promote healing of skin ulcers.
Depending on the location and extent of the involvement, a variety of techniques can be used. When deep venous reflux is mild, saphenous vein ligation can eradicate the reflux in the femoral vein and achieve skin ulcer healing. However, if the reflux is severe, direct surgery of the deep system will be required. Valve repair achieves high healing rates, in some studies similar to those obtained in primary valve repair (60% absence of recurrence at 5 years) (Raju, 1996). However, the potential thromboembolic complications of this technique limit its use.
Preventive measures:
Given the absence of effective treatments for manifestations of post-thrombotic syndrome, prevention is essential.
Elastic compression stockings are the prevention measure considered most effective at present, with a 50% reduction in post-thrombotic syndrome. These data are the conclusion of 2 clinical trials with the use of compression therapy for 24 months (Brandes, 1997; Prandoni, 2004). A recent clinical trial suggests that there is no benefit from wearing compression stockings (Kahn, 2014). However, these findings may be due to the high rate of non-compliance due to the discomfort of wearing compression stockings. The optimal indication and duration of compression therapy remains to be defined (Ten Cate-Hoek, 2010).
References
Andreozzi GM. Am J Cardiovasc Drugs. 2012 Apr 1;12(2):73-81.
Torres R. Clínica y diagnóstico diferencial de la trombosis venosa profunda y del síndrome postrombótico. In: Güell J, Rosendo A, editors. Enfermedad Tromboembólica venosa ( E.T.E.V.). Síndrome Postrombótico. Barcelona: EDIKA MED; 1995, p. 21-46.




