The term dermatoporosis was proposed in 2007 to include the different manifestations and complications of chronic skin insufficiency, also called skin fragility syndrome.1
Chronic cutaneous insufficiency consists of a set of changes inherent to the physiological process of ageing. Consequently, it is an increasingly frequent problem in our wound clinics. While Reading this post, you may think of more than one patient with recurrent wounds in the legs that are not explained by venous insufficiency, arteriopathy, occlusive vasculopathy or vasculitis, but by fragility in the context of extremely thin skin. Sun damage, topical or systemic corticosteroid treatment and anticoagulant treatment are exacerbating factors of chronic skin failure.
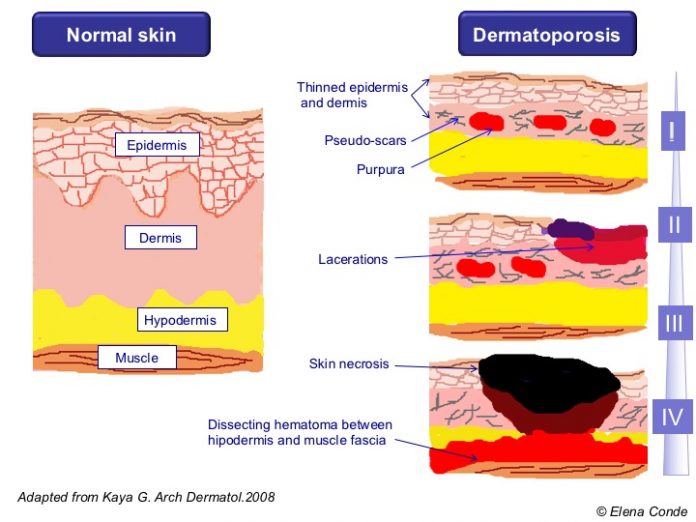
The first manifestations usually appear from the age of 60 and the evolution is progressive, with greater prevalence in the population of more than 70 years. Since clinical presentation of this pathology is variable, a clinical classification has been established with a division into 4 overlapping stages:
– Stage I: thinning of the dermis and epidermis (cutaneous atrophy), senile purpura (vascular rupture due to fragility of the vessel wall), stellate pseudo scars (loss and degeneration of collagen and elastic fibres).
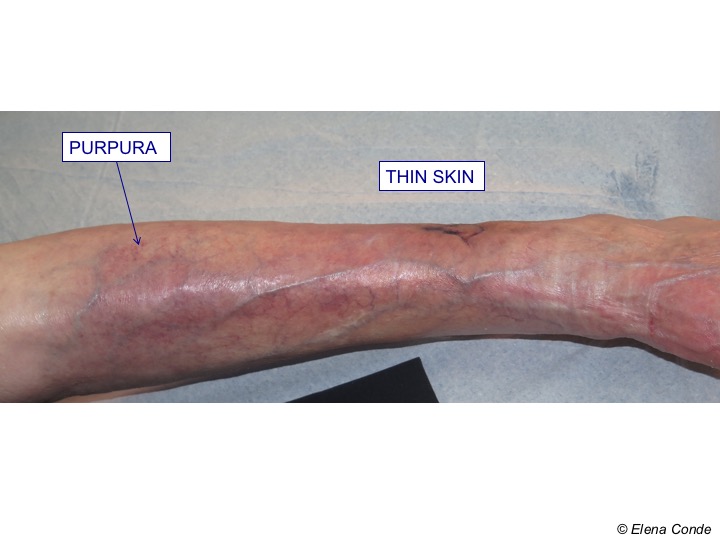
– Stage II: lacerations secondary to minor trauma are added to the previous features

– Stage III: lacerations are more extensive and recalcitrant

– Stage IV: development of a deep dissecting hematoma in the virtual space between subcutaneous cellular tissue and muscular fascia, which can produce ischemia and overlying cutaneous necrosis.


Deep dissecting hematoma represents the highest degree of expression of dermatoporosis. Early diagnosis and proper management are essential to avoid potential complications and prolonged admissions. In a series that includes 34 patients, all with leg involvement, female sex was the most affected (more than 85%) and the mean age was 81.7 years.2 The most severe cases occurred in patients treated with systemic corticoids and half of the patients were on anti-platelet or anticoagulant treatment.
The development of deep dissecting hematoma is secondary to minimal trauma. This is due to the fact that the vessels of the subcutaneous cellular tissue have a fragile wall and the skin, due to its atrophy, does not play its previous protective role. Its onset can be confused with cellulitis, as it presents with erythema, oedema and local heat. If the haematoma is not drained in this first phase, cutaneous ischemia occurs and extensive necrotic areas appear. At this stage, differential diagnosis must include the group of occlusive vasculopathies. In order to rule them out and support the diagnosis of dissecting haematoma, imaging tests (ultrasound or magnetic resonance imaging), skin biopsy (in which the subcutaneous location of the haematoma and degeneration of the dermis and vascular walls are seen) and blood tests with coagulation and autoimmunity profile are useful.
Treatment at this advanced stage would consist of surgical debridement of the necrotic plaque. Although conventional treatment is an option, to accelerate the healing process, the optimal alternative would be the use of negative pressure therapy to stimulate granulation and subsequently coverage with autologous graft.
In addition to this series, isolated cases have been published, in which you will find photos with the characteristic clinical presentation.3
Now let’s go to the practical issue: How to handle wounds in legs with dermatoporosis?
The first stage is the protection to prevent the appearance of new wounds.
In local treatment, preservation of the perilesional skin has to be prioritized, therefore scrubbing during cleansing has to be avoided and the use of atraumatic dressings is fundamental. With regard to the use of barrier products, those that leave the minimal residue should be used to avoid damage to the epidermis during cleansing for removal. It is necessary to avoid direct contact of the skin with laminated cotton bandages, since many times the epidermis is apparently preserved but in reality it presents micro-erosions to which these fibres can adhere and, with their removal, more damage can be produced.
Our clinical experience with Lipido- Colloid Technology (TLC) dressings is very good. In bleeding lesions our dressing of choice is alginate, which we also use as a secondary dressing in case of very exudative wounds. In non-exudative superficial lesions, hyaluronic acid cream is a very good choice.
What is your experience with this disease?
References
- Kaya G, Jacobs F, Prins C, Viero D, Kaya A, Saurat JH. Deep dissecting hematoma: An emerging severe complication of dermatoporosis. Arch Dermatol. 2008; 144: 1303-8.
- Gamo R, Vicente J, Calzado L, Sanz H, López-Estebaranz JL.Deep dissecting hematoma or stage IV dermatoporosis. Actas Dermosifiliogr 2010;101:89-90.http://www.actasdermo.org/es/hematoma-profundo-disecante-o-estadio/articulo/S000173100900012X/4. Inokuchi S, Nobeyama Y, Itoh M, Nakagawa H. A case of deep dissecting hematoma: different managements resulting in similar outcomes. Int J Dermatol. 2016 Dec;55(12):e628-e629.